Imagine this: you’re in the middle of a busy day, and suddenly, you feel an urgent need to use the bathroom. You rush to the toilet, only to find that you can’t seem to go. You strain and push, but nothing happens. Frustration sets in, as this feeling of being “blocked” has become increasingly common. This scenario illustrates a common struggle, and it might be linked to a condition called pelvic floor dysfunction.

Image: www.researchgate.net
The pelvic floor is a group of muscles that form a sling at the base of your pelvis. These muscles play a vital role in supporting your bladder, bowel, and uterus. When these muscles become weak or overactive, it can lead to a whole range of issues, including bowel problems. Pelvic floor dysfunction (PFD) is a prevalent condition that affects many individuals, often silently. Understanding the connection between PFD and bowel problems is crucial for addressing discomfort and achieving better overall health.
What is Pelvic Floor Dysfunction?
The pelvic floor muscles are a complex network that works tirelessly, ensuring proper bladder and bowel function. When there’s a disruption in the strength and coordination of these muscles, it can lead to PFD.
PFD can manifest in various ways, including:
- Overactive pelvic floor: This occurs when the muscles become overly tight, leading to difficulties with urination or bowel movements.
- Weak pelvic floor: This signifies that the muscles are not strong enough to support bladder and bowel function, resulting in incontinence.
- Coordination issues: This involves the pelvic floor muscles not working together properly, causing problems like urgency, frequency, or incomplete emptying.
How Can Pelvic Floor Dysfunction Affect Bowel Function?
Pelvic floor dysfunction is connected to several common bowel issues. Here’s how:
1. Constipation
The pelvic floor muscles play a critical role in bowel movements. When the pelvic floor muscles are too tight, they can hinder the passage of stool, leading to constipation. The muscles might not relax enough to allow for proper bowel emptying, leading to feelings of being “blocked.”
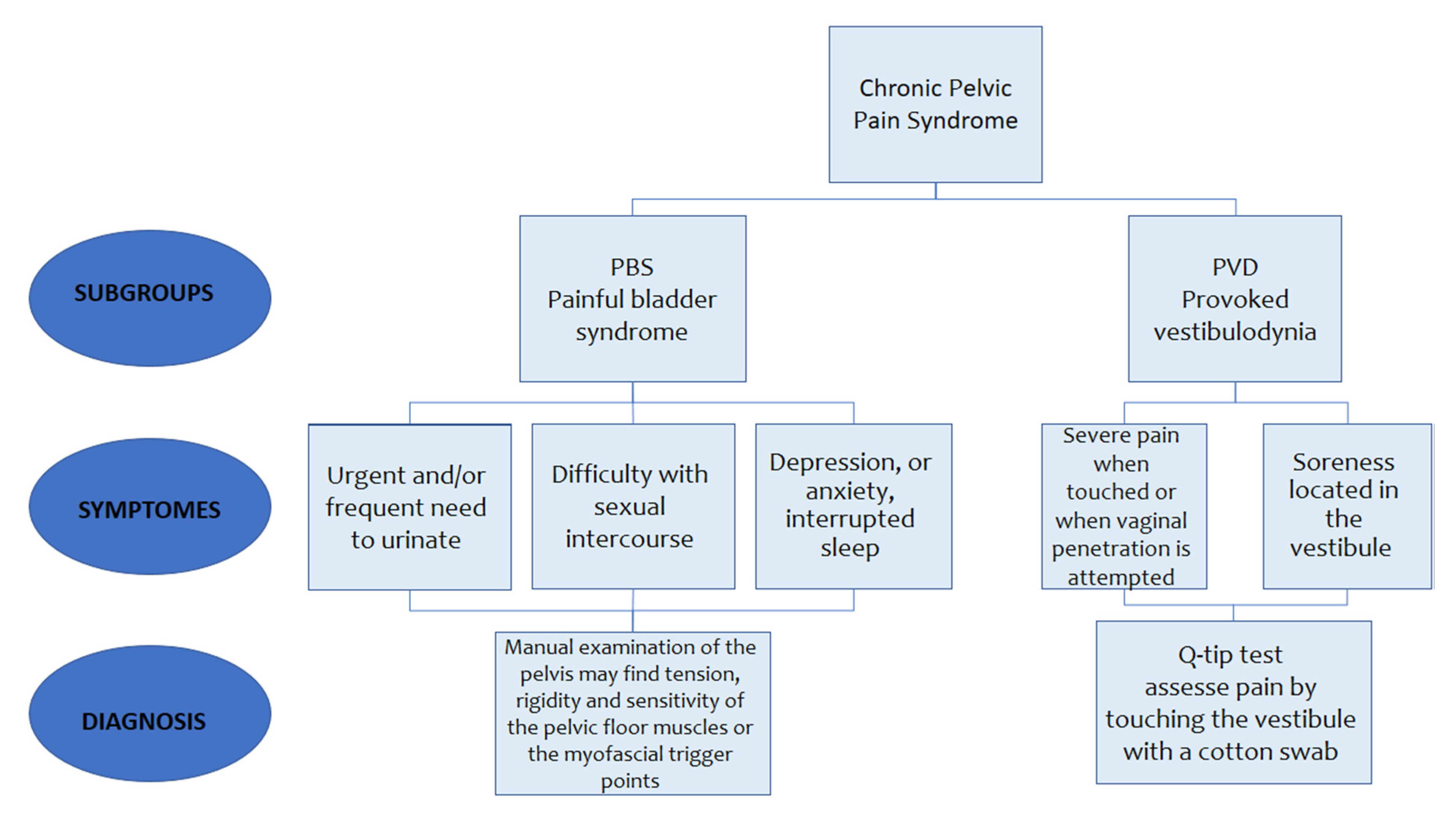
Image: viewfloor.co
2. Diarrhea
Conversely, a weak pelvic floor can contribute to diarrhea. If the pelvic floor muscles are not strong enough to control the anal sphincter, this can result in involuntary bowel leakage, particularly during periods of stress or exertion.
3. Fecal Incontinence
In extreme cases, PFD can lead to fecal incontinence, which is the involuntary loss of stool. This can be a distressing and embarrassing condition that can significantly impact quality of life.
4. Difficulty Emptying the Bowel
Another common symptom of PFD is difficulty emptying the bowel. This can feel like a sensation of being “stuck” or incomplete bowel movement. This issue could be due to the pelvic floor muscles being overly tight or not coordinated effectively during bowel movements.
Underlying Causes and Identifying Factors
Understanding the root cause of PFD is essential for developing effective treatment strategies. Some common contributing factors include:
- Pregnancy and childbirth: Pregnancy puts significant stress on the pelvic floor muscles, and childbirth can further contribute to their weakness.
- Age: As we age, the pelvic floor muscles naturally lose some strength and elasticity.
- Chronic constipation: Straining during bowel movements can overwork and weaken the pelvic floor muscles.
- Obesity: Excess weight can put added pressure on the pelvic floor muscles.
- Neurological conditions: Some neurological conditions can affect the nerve signals that control the pelvic floor muscles.
- Surgery: Pelvic surgery, especially surgeries related to the reproductive organs, can weaken the pelvic floor muscles.
- Lifestyle factors: Activities like prolonged sitting, lack of exercise, and poor posture can contribute to pelvic floor dysfunction.
Diagnosing Pelvic Floor Dysfunction
Identifying PFD often involves a thorough medical history, physical exam, and sometimes further testing. A healthcare professional will usually ask about your bowel habits, symptoms of pain, and any other relevant medical conditions.
The physical exam will involve a manual examination of the pelvic floor muscles. This may feel a little uncomfortable but is a crucial aspect of diagnosis.
In some cases, additional tests may be ordered to rule out other conditions or provide a more comprehensive understanding of the issue. These tests could include:
- Pelvic floor muscle assessment: A specialist can assess the strength and coordination of the pelvic floor muscles.
- Anorectal manometry: This test measures the pressure within the rectum and anus, helping to diagnose conditions like constipation or fecal incontinence.
- Colonoscopy: This procedure involves inserting a thin, flexible tube with a camera into the colon to visualize the lining. It can reveal any abnormalities that might contribute to bowel dysfunction.
Treating Pelvic Floor Dysfunction
Treating PFD involves addressing the underlying cause and improving the function of the pelvic floor muscles. Here are some common treatments:
- Pelvic floor muscle exercises (Kegels): These exercises help to strengthen and improve the coordination of the pelvic floor muscles.
- Biofeedback therapy: This involves using sensors to monitor muscle activity and provide feedback on how to improve muscle control.
- Manual therapy: A physical therapist can use manual techniques to release tension in the pelvic floor muscles and improve their function.
- Lifestyle changes: Making adjustments to diet, exercise habits, and stress management can help to manage PFD.
- Medications: In some cases, medication may be used to address constipation or other symptoms.
- Surgery: In rare cases, surgery may be considered for more severe cases of PFD.
Lifestyle Modifications for a Healthier Pelvic Floor
Making positive changes to your lifestyle can significantly benefit your pelvic floor health. Here are some practical tips:
- Dietary changes: Increase your fiber intake by incorporating more fruits, vegetables, and whole grains into your diet. Stay hydrated by drinking plenty of water throughout the day.
- Regular exercise: Engage in moderate-intensity exercises like walking, swimming, or yoga, which can help improve pelvic floor strength and coordination.
- Proper posture: Pay attention to your posture while sitting and standing, ensuring your core muscles are engaged to support the pelvic floor.
- Stress management: Chronic stress can significantly impact the pelvic floor muscles. Practice relaxation techniques like deep breathing, meditation, or yoga to manage stress levels.
Expert Insights and Actionable Tips
Dr. Susan, a renowned pelvic floor therapist, emphasizes the importance of early intervention: “Don’t ignore changes in your bowel habits or discomfort in the pelvic region. seeking evaluation and treatment can prevent PFD from progressing and potentially causing more significant issues.”
Dr. John, a gastroenterologist, highlights the role of a multidisciplinary approach: “Collaborating with a pelvic floor therapist, a gastroenterologist, and other healthcare providers as needed is crucial for comprehensive management of PFD-related bowel problems.”
Can Pelvic Floor Dysfunction Cause Bowel Problems
Conclusion
Navigating the complexities of pelvic floor dysfunction and its impact on bowel health can be overwhelming. But through understanding the intricate connection between these systems, you can empower yourself with knowledge and actionable steps. Don’t hesitate to seek guidance from a healthcare professional for personalized assistance in managing your condition. Remember that taking proactive steps to address pelvic floor dysfunction can lead to improved bowel function, increased comfort, and ultimately, greater quality of life.






